What Are Delirium Tremens?
Delirium Tremens Explained
More commonly known as the DTs, most people know delirium tremens signify alcohol withdrawal. There’s a lot more to delirium tremens symptoms than shaking. Many people experience hallucinations, a racing heart, and sweating.
Here, we take an in-depth look at how the symptoms of delirium tremens appear. Also, who suffers from them, how to avoid them, and the associated risks and dangers.
What are Delirium Tremens Symptoms?
The symptoms can range from mild to severe and last for up to 3 days on average. In the most severe delirium tremens, you can die if not treated.
- Confusion – they may be confused by what is happening to them, unable to answer simple questions, suffer from disorientation, detachment from reality.
- Shaking – Uncontrollable shaking that is especially evident in the hands.
- Sweating – Resulting from the body not regulating temperature, hot and cold flashes, fever, and the body trying to expel alcohol quicker through sweat.
- Shivering – Unable to self-regulate body temperature, developing a fever.
- Irregular heart rate – Heart rate may race uncontrollably, palpitations or skip beats.
- Hallucinations – Seeing and hearing things that are not there. Naturally, this will add to the symptoms of confusion.
- Very high body temperature and seizures – alcoholic seizures are extremely dangerous.
Any person who develops delirium tremens must seek URGENT medical attention at their local hospital to avoid coma and death.
Causes of delirium tremens
Drinking alcohol frequently and excessively changes how our brain works. Our brain’s GABA levels control how relaxed and anxious we are. Alcohol works so that it imitates GABA and binds to the same receptors. This makes us feel temporarily calm and happy.
Alcohol also slows down the part of our brain that gets us excited and anxious Glutamate. Dopamine, the reward chemical of our brain, increases, giving us a temporary feel-good factor.
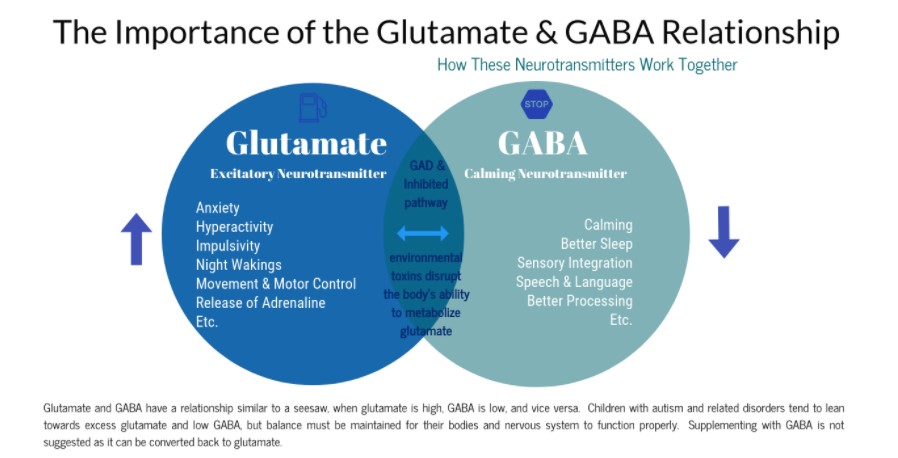
Slowly as we take alcohol too regularly, though, our body adjusts. It produces less GABA and dopamine and more Glutamate. This means that when we stop taking it, we no longer compensate for these parts of our brain. It sends our body into a state of withdrawal.
This causes several alcohol withdrawal symptoms to manifest.
In cases of minor alcohol withdrawal less severe symptoms such as anxiety, nausea, insomnia, sweating and tremor occur. Acute alcohol withdrawal symptoms are more dangerous such as seeing and hearing things that are not there.
Who is at risk of the DTs?
Anyone who is physically addicted to alcohol is at risk of developing DTs. This is especially true of those that suffer from chronic alcoholism. Whilst delirium tremens are quite rare. Still, an estimated 10-15 % of alcoholics will experience them.
Attempting to go ‘cold turkey’ from alcohol addiction and stopping abruptly without medical intervention can be catastrophic. We would strongly recommend a medical alcohol detox for your safety.
Developing DTs is most common in alcoholics who have detoxed and started drinking again. The more detoxes a person does, the higher their risk of developing complications such as delirium tremens.
The risk is higher if you are:
- In poor physical health
- Addicted to drugs
- Have a history of seizures
- Have been addicted to alcohol for a long time
Identifying Delirium Tremens
Spotting the symptoms of DTs in someone you care for could save their life if you take the appropriate action quickly.
The most common symptom of delirium tremens is commonly referred to as the “Shakes”. Look out for:
- A tremor that they cannot control.
- Tremor worst in the extremities (hands and legs).
- They cannot walk or hold a cup.
- Trembling as they talk.
- A jittery tone to their voice.
- Other signs of delirium tremens you can see are:
- Acting confused frequently.
- Seeming clumsy or lost when sober.
- Seeing things or talking to people who aren’t there.
Drinking more alcohol may temporarily help to alleviate the symptoms, but this method is not guaranteed. These symptoms can become life-threatening if not immediately and appropriately seen by a doctor.
If your loved one or family member is drinking daily and heavily or has previously displayed any signs of alcohol withdrawal. They will need professional medical help to stop drinking alcohol safely.
Risks of Delirium Tremens
The biggest danger and risk associated with developing delirium tremens is death. Delirium tremens carry a 15% mortality rate with treatment and up to 35% mortality rate without treatment.
Experiencing repeated delirium tremens and seizures can also lead to alcohol-related brain damage, alcoholic delirium psychosis and the onset of Wernicke-Korsakoff syndrome.
Avoiding Delirium Tremens
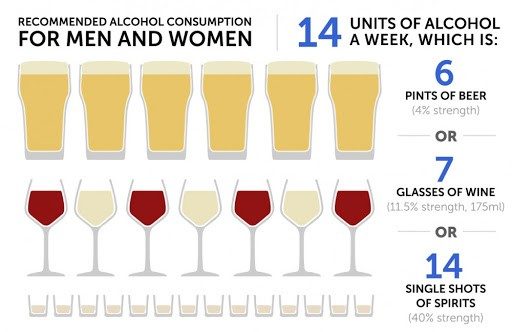
The most effective way of preventing the onset of delirium tremens is to keep your drinking within the Chief Medical Officers’ Safe Drinking Guidelines.
If you have an alcohol dependence, you mustn’t quit drinking suddenly. You will need medical detox.
A standard alcohol detox programme in an inpatient clinic is managed over 7-10 days. We do not recommend attempting this by yourself at home. Numerous risks and complications can arise with medication if not fully medically supervised.
Rehab Guide provide safe and effective medical detoxes for alcohol within our CQC registered detox clinics and rehab centres. All medical alcohol detoxes are carried out by our qualified doctors, nurses and highly skilled therapists. We provide medical and therapeutic care around the clock to ensure that each patient’s detox is as safe and as comfortable as possible, with minimal risk to their health.
Treatment for Alcohol Abuse and Addiction
Delirium tremens treatment and delirium tremens medication are available on prescription. The most common are benzodiazepines. Benzodiazepines help relax the body and brain during detox and have a sedative effect. This replaces the alcohol in the body without blocking the chemicals in the brain.
Allowing your body time to recover naturally from stopping drinking should prevent delirium tremens.
If you wish to stop drinking alcohol but cannot afford an inpatient alcohol detox, you have the option of a home detox or GP referral.
Sources and references:
- Primary Care Companion to the Journal of Clinical Psychiatry. doi:10.4088/PCC.10r00991ecr. PMC 2947546. PMID 20944765.
- “Recognition and management of withdrawal delirium (delirium tremens)”. The New England Journal of Medicine. 371 (22): 2109–13.
- https://emedicine.medscape.com/article/166032-overview.
- NICE Clinical Guidelines, No. 100. National Clinical Guideline Centre (UK).





